HIV change blocks treatment plan
Photo/FILE
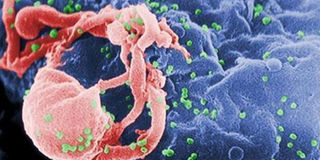
New mutant strains could compromise the gains made against HIV.
The Aids virus is blocking efforts to provide all infected Kenyans with anti-retroviral drugs, according to new evidence.
Mater and Coast General hospitals have discovered that after being exposed to anti-retrovirals for some years, the virus has changed (mutated) with most new infections not reacting to common drugs.
According to local and international medical researchers who investigated newer infections in six African countries, new mutant strains could compromise the gains made against HIV.
The study published on Thursday in the medical journal, The Lancet, was conducted by the two hospitals.
The medical researchers looked at the virus among newly infected people who had not used anti-retrovirals and found strains that were already drug resistant, which means some hard-to-treat strains have appeared.
Although this has been suspected for some time there was no evidence on how widespread the mutant strains are in the region.
The study associated extensive use of anti-retrovirals with the emerging resistant strains in Africa.
New medicine
Ideally Kenya should adopt new and more effective medicines but this could be expensive, according to the head of the National Aids/STD Control Programme (NASCOP), Dr Nicolas Muraguri.
“The alternative is to improve patient monitoring and their adherence to doctors’ instructions in the short term.”
The research focused on groups of HIV-infected adults since 2007 who had not started anti-retroviral treatment from 11 regions in Kenya, Nigeria, South Africa, Uganda, Zambia and Zimbabwe.
Uganda was found to have the highest HIV drug resistance rate at 12.3 per cent, South Africa1.1 per cent and Kenya 4.9 per cent in Mombasa and 4.5 per cent in Nairobi.
The researchers say the higher drug resistance in Uganda could be related to early start of ART in the country in the 1990s compared to Kenya where the treatment was accelerated almost four years ago with close to 450,000 HIV positive people being covered now.
The risk of primary resistance in a region, was found to increase by 38 per cent for each additional year passed since the start of the local anti-retroviral roll-out.
“Our findings support the hypothesis that widespread distribution of anti-retrovirals in Africa is driving the emergence of primary drug resistance, which has public health implications,” the report stated.
This situation is different in developed countries which have newer and more effective drugs, consistent medicine supply and good patient monitoring.




