Nine million to get free health cover in NHIF plan

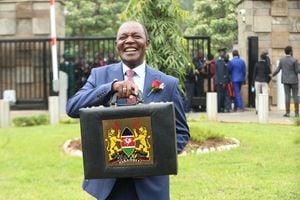
Medical Services minister Prof Anyang’ Nyong’o (right) and the NHIF CEO Simeon Ole Kirgotty at a news conference in Nairobi last month, where they said the revised contribution rates would take effect from this month. The plan has since been contested in court. Below: NHIF offices.
What you need to know:
- A pilot of NHIF Health Insurance Subsidy Programme will be carried out next month to provide baseline information
- Specifications will be developed to meet the requirements for hospitals and clinics among others
Nine million poor Kenyans will benefit from free healthcare next year following a new programme spearheaded by the national health insurer.
The National Hospital Insurance Fund (NHIF), with sponsorship from the Rockefeller Foundation amounting to Sh23 billion, will roll out a health package for the poor that will include general consultation, laboratory tests, drugs and X-rays for free.
Other services to be extended include diagnosis and treatment of common ailments, ear-nose-and-throat (ENT) services, HIV, diabetes, asthma among other chronic diseases, diagnosis and clinical counselling, a report of the scheme notes.
A pilot of NHIF Health Insurance Subsidy Programme will be carried out next month to provide baseline information, including a network of hospitals — public, private or faith based — before the roll out in February and July respectively.
The Fund’s Strategy and Planning manager Marua Chacha said beneficiaries will be integrated into NHIF registration platform and a biometric system would be used to identify them at the hospitals that will be earmarked to provide the services.
Specifications will be developed to meet the requirements for hospitals and clinics among others, the subsidy programme report states.
“This is part of global and national initiative to enable the vulnerable segments of the population to access quality health care,” Mr Chacha said.
He said the target group is to be drawn up by the Ministry of Gender Children and Social Development through the social protection programme that uses indicators to identify the poor.
“This population does not have any form of health insurance and are left with the costly option of direct purchase to meet their health care,” Mr Chacha said.
According to the report, about 20 per cent of the population lives below the poverty line.
“The health system in Kenya is unbalanced and under-funded with 28 per cent of total health expenditure paid directly from out-of-pocket expenditure.” Read (Court extends order halting roll-out of higher NHIF rates)
These direct payments deter the us of medical services by the poorest — estimated at 9 million — and as a result their health needs are deferred.
The out-of-pocket expenditure is characteristic of the poor who are unable to pre-pay for their future health needs and as such are not a priority.
This has seen about 100,000 families pushed below the poverty line by the direct payments, it states.
But on the other hand, the highest end of the population have high disposable incomes which allows for choice with regard to financing future health needs.
According to Medical Services minister Anyang’ Nyong’o, only enhanced contributions to the NHIF will meet quality healthcare needs of the citizens.
Already the proposed contributions where the highest paid contributes Sh2,000 per month, and are being contested in court, were said to be still little for quality healthcare.
The NHIF said deductions ranging between Sh400 and Sh3,885 would meet the required standards.
“This is why I emphasise that the health sector should not be characterised by an overstretched public sector and an under-utilised private sector including the faith-based organisations,” Prof Nyong’o said.
Among other plans to achieve this, the NHIF wants to dispose of its Sh12 billion assets in plans to re-focus management on core business of providing health services.
The Fund is also contemplating hiving off its deductions wing and contracting an agency to carry out the task in plans that will free it to concentrate on purchasing healthcare, among other proposals.
“The role of the NHIF will then be restricted to service provision,” Mr Chacha said, adding that the first of this step has been to recruit managers who are trained in particular skills.
“This will revamp and transform the fund while enhancing competition to provide quality and affordable healthcare to the contributors,” acting NHIF chief Simeon Ole Kirgotty added.
Boosting liquidity
But Mr Chacha noted that boosting the liquidity of the fund served to provide essential services as opposed to owning assets that did not enable NHIF meet such objectives.
For instance, Mr Chacha told the forum that NHIF in Taiwan had 94 per cent of its worth in form of other investments as opposed to Kenya’s whose fortunes were holed up in fixed assets.
The World health Assembly in 2005 adopted the resolution that urges countries to develop their health financing systems to provide all people with access to needed health services.
Such services, the assembly said, should be of sufficient quality to be effective and ensure that the use of these services does not expose the user to financial hardship.
In anticipation of this resolution, the Ministry of Health had earlier introduced a temporary measure that medical care at dispensary and health centre level would be free, although a minimal co-payment in government institutions for administration would be extended.
A health card for the poor to allow free access to health services was to be financed through a proposed tax system.
But this did not materialise due to lack of political goodwill, budgetary constraints, and lack of transparent decision-making among other challenges, the NHIF report said.
This situation was worsened by the fact that only 10 per cent of the population has health insurance, with NHIF covering 20 per cent of this population.
Poverty rate in Kenya is estimated at 46 per cent with 19 per cent of the proportion of the population living in absolute poverty.
Such poverty is hard to reverse due to its inter-generational and multifaceted nature and is characterised by persons, who have no access to productive assets, education, healthcare, income, food, decent housing and clothes among others.
“Poor health and health-related expenses constitute the most often stated reason for households’ declining into poverty,” it states.
About 73 per cent of households that have fallen into poverty mentioned sickness, poor health, and heavy healthcare expenses as a principal reason for their decline into abiding poverty.