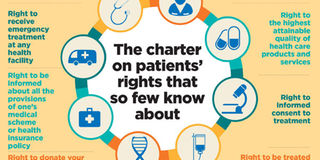
The charter on patients’ rights that so few know about
What you need to know:
- Elizabeth Merab spoke to Tabitha Griffith, a legal officer at the Kenya Legal and Ethical issues Network on health (KELIN), who provided insights into the 2013 patients’ rights charter.
Alex Madaga’s story is probably one of the stories that people will remember for a long time.
Madaga, an accident victim, spent 18 hours in an ambulance because Kenyatta National Hospital in Nairobi said it did not have a free ICU bed to admit him.
And despite bleeding in his brain, the patient could not be taking in by private hospitals without a cash payment of Sh200,000.
Mr Madaga, who later died at KNH’s ICU while undergoing treatment, started receiving treatment a day later, after his family reportedly protested to have him admitted at the referral hospital.
Sadly, while Madaga’s case, might be extreme, such cases are common.

Relatives visit Mr Alex Madaga at Kenyatta National Hospital's ICU on October 8, 2015. Alex Madaga’s story is probably one of the stories that people will remember for a long time. PHOTO | JEFF ANGOTE | NATION MEDIA GROUP
Barely a month after his story was published in the Daily Nation, another one was that shocked the nation occured.
Elizabeth Akala, who was pregnant, was reported to have died after medical staff clocked out at the end of their shift, leaving her unattended, crying in pain and begging for help for 14 hours at the Kakamega Provincial General Hospital.
Her family said that although Ms Akala had been examined and seen to be an emergency case, nurses and doctors in the labour ward signed off at the end of their shift and only returned the next day, when her condition had worsened.
“The gynaecologist then admitted her and told us that she was too tired and had completed her shift, in fact, she told us that she had even overstayed by more than an hour...,” Mr Zacharia Ludenyo, her husband, told the Nation at the time.
Amidst all these unfortunate instances, one thing remains clear: most patients are not conversant with the Patients’ Rights charter.
The first edition of the Kenya National Patients’ Rights charter was launched two years ago (2013) by the Ministry of Health.
It is meant “to inform clients and patients of their rights and responsibilities, thus empowering them to demand quality services from health care providers.”
“The Ministry of Health expects all healthcare providers to be familiar with the charter and apply it diligently in the provision of health care services,” reads the executive summary of the charter.
Despite outlining the rights that every patient is expected to exercise, legal and human rights activists feel that much should have been done to educate the masses on the document and make them aware of the rights they have when it comes to attain the best health care.
RIGHT TO ACCESS HEALTH CARE
Ms Tabitha Griffith describes this first right as a fundamental right under which every other right falls.
According to the charter, every person should be able to access promotive, preventive, curative, reproductive, rehabilitative and palliative care without straining.
To access health care, the facility must be within the patient’s reach.
“This right also allows you, as a patient, to access health care without discrimination or stigma whatsoever,” she says.
RIGHT TO RECEIVE EMERGENCY TREATMENT AT ANY HEALTH FACILITY
In the recent past, questions have been raised regarding this right following the death of patients who could not get admission to health facilities because they could not pay deposits.
Often, hospitals ask for a deposit even when it is an emergency. But the rights’ charter reaffirms and wants patients to understand that they have a right to access emergency treatment, with or without money.
“Any patient who has been determined by health professional to be in need of emergency treatment should receive treatment to stabilise them irrespective of their ability to pay.”
RIGHT TO BE INFORMED ABOUT ALL THE PROVISIONS OF ONE’S MEDICAL SCHEME OR HEALTH INSURANCE POLICY
You are entitled to know all the privileges accorded to you by your health insurer.
This includes the contents and decisions of the medical scheme and health insurance policy.
You are, therefore, advised to always read the terms and conditions of your insurance cover.
However, this is one of the rights that is difficult to exercise. In fact, Ms Griffith argues that this is more or less a right that exists only on paper as it is often ignored by insurance companies.
You also have a right to insurance coverage without discrimination on the basis of age, pregnancy, disability or illness (including mental disorders).
RIGHT TO DONATE YOUR ORGANS OR ANY OTHER WISHES UPON YOUR DEMISE
While you have a right to donate your organs, this right can only be exercised if the Health Bill becomes law.
RIGHT TO BE TREATED WITH RESPECT AND DIGNITY
This right is drawn from Article 28 of the constitution, which states that every person has inherent dignity and the right to have that dignity respected and protected.
RIGHT TO CHOOSE A HEALTH CARE PROVIDER
While this right gives you the right to choose the doctor or nurse you would want to treat you, Ms Griffith notes that it is often abused by some health workers, who take advantage of patients’ ignorance.
“We have had cases of patients going to particular hospitals because they have been referred to see a particular doctor. However, they end up in a different doctor’s office altogether because the receptionist did not think that they have a right to choose whom they want to see,” she explains.
This right is also hard to exercise in public hospitals where, Ms Griffith says, human resources are overstretched.
RIGHT TO THE HIGHEST ATTAINABLE QUALITY OF HEALTH CARE PRODUCTS AND SERVICES
You have a responsibility to confirm that the products and services you are receiving are of the best.
Do not accept expired drugs and always verify the expiry date of the medicines you are given.”The government also has a responsibility to dispatch drugs on time.
RIGHT TO CONFIDENTIALITY
While every person has a right to have their medical information kept confidential, this right, Ms Griffith notes, is often breached by health workers.
“Confidentiality shall be upheld except where consent has been expressly given or disclosure is allowed by law or in the public interest. Confidentiality should be maintained even after the patient dies,” states the charter.
RIGHT TO INFORMATION
Subsequently, you should be able to access your medical record without any hitches should there be a need for you to do so.
According to Ms Saoyo, this is the most contentious right in the charter as it is often violated.
“We have had a number of cases where patients’ records have gone missing from the hospitals where they were being treated and you wonder how these records would just go missing when they are needed.”
RIGHT TO A SECOND MEDICAL OPINION
You have a right to a second opinion about your diagnosis, procedures and treatment to undergo, if you so wish.
“If you think or feel that you have been misdiagnosed, you should seek a second opinion. Sometimes doctors do make mistakes. Always seek a second — or even third — opinion if possible,” advises Ms Saoyo.
RIGHT TO INFORMED CONSENT TO TREATMENT
You have a right to be given accurate information about your health status in a language that you can easily understand, the charter states.
“This is not merely about the doctor seeking the patient’s permission to perform a procedure,” says Ms Griffith. “You should be informed of the nature of your illness and taken through the risks, the diagnostic procedures, proposed treatment, alternative treatment and the costs involved.”
The decision thereafter should be made willingly and free from duress.
RIGHT TO COMPLAIN
The charter notes that you have a right to complain about the health services of any health facility to the relevant authorities and have such complaints investigated and a response from the authority received within 12 months (one year), Ms Griffith says that many patients are not even aware of this provision.
RIGHT TO REFUSE TREATMENT
The charter notes that any person, patient or client may refuse, withdraw or withhold treatment provided it does not create an immediate danger to them or the health of other people.
However, it states that such refusal shall be documented in writing by the medical service provider in the presence of an independent witness.
This right can also be limited if it is constitutionally thought to be at variance with public health concerns.





