Factsheet : Hysteroscopy
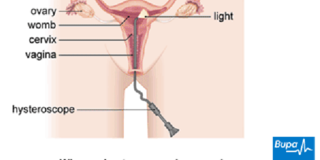
Where a hysteroscope is passed Picture Bupa Health
What you need to know:
- A hysteroscopy is a procedure that allows a surgeon to look inside the womb (uterus) using a narrow tube-like telescopic camera called a hysteroscope.
- A hysteroscopy can be used either to diagnose or treat a gynaecological condition.
A hysteroscopy is a procedure used to examine the inside of your womb. It can be used either to diagnose or to treat a gynaecological condition. You surgeon may carry out a hysteroscopy to:
• help find out what is causing your symptoms, for example if you have heavy periods
• check for conditions such as polyps (small growths of tissue in your womb lining) or some types of fibroids (non-cancerous growths of muscle in your womb)
• see if there are any problems within your womb if you're having problems getting pregnant or have had several miscarriages
• treat scar tissue (adhesions) within the lining of your womb
• put in an intra-uterine system (IUS), or coil, or take out a coil that has moved out of place
• carry out a permanent form of contraception
WHAT ARE THE ALTERNATIVES?
Depending on your symptoms and circumstances, there may be alternative treatments or investigations available to you.
A pelvic ultrasound scan can be used to diagnose some gynaecological conditions. An ultrasound scan uses sound waves to produce an image of the inside of your womb.
Other types of scan, such as an MRI or CT can sometimes be used.
An endometrial biopsy is an alternative to a hysteroscopy if your surgeon needs to take a sample of the lining of your womb.
A narrow tube is passed through your cervix and into your womb, then gentle suction is used to remove samples of your womb lining that will be examined under a microscope. Sometimes you may have this at the same time as a hysteroscopy.
Your surgeon will explain the different options to you.
PREPARING FOR A HYSTEROSCOPY
Your surgeon will explain how to prepare for your procedure. For example, if you smoke you will be asked to stop, as smoking increases your risk of getting a chest infection and slows your recovery.
Hysteroscopy used for diagnosis is usually done as an outpatient procedure. This means you don’t need to stay in hospital overnight and may not need anaesthesia.
Your surgeon may suggest that you take a painkiller such as paracetamol (acetaminophen) about half an hour before your appointment.
Alternatively, you may have the procedure as a day-case under general anaesthesia, which means you will be asleep during the operation. If you're having a general anaesthetic, you will be asked to follow fasting instructions.
This means not eating or drinking, typically for about six hours beforehand. However, it's important to follow your surgeon’s advice.
At the hospital, your nurse may do some tests such as checking your heart rate and blood pressure, and testing your urine.
Your surgeon will discuss with you what will happen before, during and after your procedure, and any pain you might have.
This is your opportunity to understand what will happen, and you can help yourself by preparing questions to ask about the risks, benefits and any alternatives to the procedure.
This will help you to be informed, so you can give your consent for the procedure to go ahead, which you may be asked to do by signing a consent form.
What happens during a hysteroscopy?
The procedure used for a diagnosis usually takes about 10 to 15 minutes. It can take about one hour if you’re having a general anaesthetic.
Your surgeon will put a medical instrument called a speculum into your vagina to see into your cervix (neck of your womb). He or she will then clean your vagina and cervix with an antiseptic solution and pass a hysteroscope into your womb.
The camera on the end of the hysteroscope sends pictures from the inside of your womb to a video screen. Your surgeon will look at these images and, if necessary, take a biopsy or carry out any treatment.
He or she may inject some gas or fluid, which can make it easier to see the womb lining.
WHAT TO EXPECT AFTERWARDS
If you have a general anaesthetic, you will need to rest until the effects have passed. One you feel ready, you will need to arrange for someone to drive you home and you should try to have a friend or relative stay with you for the first 24 hours.
General anaesthesia can temporarily affect your coordination and reasoning skills, so you should not drive, drink alcohol, operate machinery or sign legal documents for 24 hours afterwards.
If you're in any doubt about driving, contact your motor insurer so that you're aware of their recommendations, and always follow your surgeon's advice.
You may need to wear a sanitary towel as the procedure can cause you to have some vaginal bleeding. If you need pain relief, you can take over-the-counter painkillers such as paracetamol or ibuprofen. Always read the patient information that comes with your medicine.
Your nurse may give you a date for a follow-up appointment. If you have a biopsy or polyps removed, the results will usually be sent in a report to your doctor.
RECOVERING FROM A HYSTEROSCOPY
If you have a diagnostic hysteroscopy, you will need to rest and take it easy for a day or two. If you have had treatment during the hysteroscopy, for example if you have had a polyp or fibroid removed, your recovery may take longer.
Your surgeon will advise you when you can get back to your usual activities.
WHAT ARE THE RISKS?
As with every procedure, there are some risks associated with hysteroscopy. We have not included the chance of these happening as they are specific to you and differ for every person.
Ask your surgeon to explain how these risks apply to you.
SIDE-EFFECTS
Side-effects are the unwanted but mostly temporary effects you may get after having the procedure. For example, you may have cramping pains, like those you get during a period.
You may also have some vaginal bleeding, which usually gets better after a few days, but can last for up to a week.
COMPLICATIONS
This is when problems occur during or after the procedure. Most women aren't affected. The possible complications of any operation include an unexpected reaction to the anaesthetic, excessive bleeding or developing a blood clot, usually in a vein in your leg (deep vein thrombosis, DVT).
Specific complications of hysteroscopy are uncommon, although it's possible you may develop an infection afterwards, which can lead to infertility – but this is rare.
The surgery may damage your womb and, rarely, your bladder, bowel and blood vessels. If this happens, you may need further surgery to repair any damage caused.
During the procedure, it may not be possible for your surgeon to pass the hysteroscope into your womb to get a clear view of the lining. If this happens, he or she will discuss alternative options with you.
You may need to have a laparoscopy (keyhole surgery) or laparotomy (open surgery) instead.
Most women don’t have any problems after having a hysteroscopy. However, if you develop any of the following symptoms, contact your doctor.
• Long-lasting, heavy bleeding.
• Vaginal discharge that is dark or smells unpleasant.
• Severe pain or pain that lasts for more than 48 hours.
• A high temperature.
Speak to your surgeon for more information about complications of hysteroscopy.
Produced by Krysta Munford, Bupa Health Information Team, October 2012.




