Restoring smiles a surgery at a time
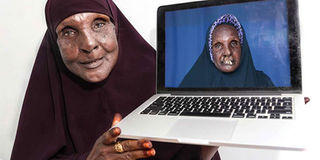
You may never appreciate the power of surgery until you see the beaming face of 56-year-old Karuuro Mohamed, who was born with a cleft lip. PHOTO| POOL
What you need to know:
- Besides being a surgeon and lecturing at the UoN’s Department of Human Anatomy, Dr Kamau runs the Bela Risu Foundation that offers free surgery services to children with cleft lips and people like Ms Mohamed who need reconstructive operations.
- “Cleft repair surgery is simple, and the transformation is immediate,” says Dr Kamau.
- Through Bela Risu, Dr Kamau is one of the medics involved in operations by Smile Train, an international charity involved in free cleft repairs across Africa.
You may never appreciate the power of surgery until you see the beaming face of 56-year-old Karuuro Mohamed, who was born with a cleft lip.
Her life changed in March 2018 when volunteer surgeons operated on her.
By the time the surgery was over, the hitherto split portions of Ms Mohamed’s upper jaw were drawn together and Ms Mohamed, a resident of Galgaduud Banaadir in Somalia, could look normal again. The operation was done at the Kalkaal Specialty Hospital in Somalia.
The before-and-after photos of Ms Mohamed tell a story of a complete makeover; the type that warms the hearts of medics. The transformation was partly due to the efforts of Dr Martin Kamau, a University of Nairobi (UoN) lecturer. Dr Kamau was born of a South Korean mother and a Kenyan father. He has more than a decade of experience in dental surgery and operating on the face, mouth and jaws of patients.
CLEFT REPAIR SURGERY
Besides being a surgeon and lecturing at the UoN’s Department of Human Anatomy, Dr Kamau runs the Bela Risu Foundation that offers free surgery services to children with cleft lips and people like Ms Mohamed who need reconstructive operations.
“Cleft repair surgery is simple, and the transformation is immediate,” says Dr Kamau.
Through Bela Risu, Dr Kamau is one of the medics involved in operations by Smile Train, an international charity involved in free cleft repairs across Africa.
“The operation takes only 45 minutes,” he says, adding that a cleft lip is milder compared to cleft palate. “In cleft lip, all the components are there: the skin and the muscles. But you have to bring all those components together. You also have to try and perfect the operation so that the lip looks perfect.”
According to Kamau, the condition affects one in every 700 births in Kenya, mostly in remote places like northern Kenya. Palate deformities, where the roof of the mouth does not unite properly, are more complex to fix than closing a clip lip. A cleft lip may require one or two surgeries, depending on the extent of the repair needed. They can conduct the first repair when the baby is around three months old.
He recalls how one of his adult patients started dancing minutes after he had finished the operation. “Through translation the gentleman who was in his fifties, he said he could now smile and started jumping up and down. I still had my scrubs on.” He explains that one may require several surgeries over a decade after the first repair of the palate, noting that the first palate surgery is best done between six and 12 months to create a functional palate, to reduce the chances that fluid will develop in the middle ears, and to help in the proper development of the teeth and facial bones.
“The condition can have a considerable impact on a child’s well-being in the early years but the outlook is normally very good. The major goals of surgical intervention are normal speech and minimising growth disturbances.”
According to the doctor, the problem in most parts of Kenya is delayed intervention, cultural issues and financing.
“Sometimes parents may not know this condition can be rectified and so they hide their children.”.
He narrates about one community in northern Kenya that has more cases than any other part in the country. A mother from the region, he says, was misled into believing that if her child’s cleft lip was repaired, all her subsequent children would also have cleft lips. She never took the child for surgery.
Children who grow with this condition learn new ways of forming words, and those with a cleft palate often speak with a nasal drawl. They have problems eating, breathing and speaking, and this carries the risk of severe malnutrition and even death for children.
Many of them cannot attend school, hold a regular job or get married.
“They face very difficult lives filled with shame and isolation, pain and heartache,” says Dr Kamau. “Even if the condition is rectified later in their life, they may never be able to re-learn speech.”
According to the medic, a single surgery can cost as much as Sh500,000 or higher, depending the hospital.
Our interview also touched on Dr Kamau’s nativity story. His mother, he said, is a naturalised Kenyan citizen from South Korea. He was initially known as Warui Kamau but he was forced to change the name.
“I had to change, or rather add Martin to my name, because every time I introduced myself as Warui Kamau no one would believe me. A teacher once punished me because she thought I was lying,” he says with a smile on his face.
He gives another example of the first time he reported to Meru Level 5 hospital, as it was known back then. The medical superintendent opened the door after the secretary had told him that a certain Dr Kamau was there to see him then immediately shut it.
“He opened the door and he looked at me, asked the secretary where Dr Kamau was before he closed it. I had to introduce myself to him,” narrates the medic.
He says he will never change the name. He adds that despite being half Korean, he has only visited the Asian country once and that is when he was young. He has given his son a Korean name but he has none himself.
His foundation, Bela Risu (which means “beautiful smile” in Portuguese) offers free cleft lip and cleft palate surgeries and highly subsidised safe surgeries from other surgical specialties, all with the aim of restoring hope and dignity to the victims.
This is achieved through the huge pool of volunteer surgeons who join them during the several surgical missions within Africa. He has done surgeries in Kenya, Somalia, Zimbabwe, DR Congo, Tanzania, Rwanda, Cameroon, India, among other countries.
On challenges he has faced while working, Dr Kamau says that lack of proper education has left many people in need surgery to live with deformities.
He adds that their work would not be possible without help from governments, mostly in the form of infrastructure and manpower.
“We coordinate with the counties after donors facilitate us with everything we need to do the surgery and the government comes in to offer their facilities, theatres and even manpower,” he says.




