Are my allergies all in my head?

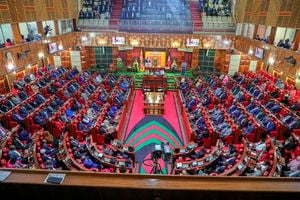
Emotional factors can make allergies better or worse. PHOTO | FILE | NATION MEDIA GROUP
What you need to know:
- While emotions and psychological stress do not cause allergies, they can worsen symptoms.
- Mind-body techniques may be useful adjuncts in easing symptoms, but they are not sufficient to treat the underlying problem.
Q: Are my allergies all in my head?
A: No. But emotional factors can make allergies better or worse.
Doctors have long suspected a connection between allergies and the psyche. In 1883, Dr. Morell Mackenzie, a pioneer in the field of ear, nose and throat medicine, observed, “It has long been noticed that attacks of prolonged sneezing are most apt to occur in persons of nervous temperament.”
In the 1940s, doctors discovered that allergic patients could be tricked into experiencing allergy attacks. In one case, a doctor exposed a patient to a goldenrod plant, without telling the patient that the plant was artificial. The patient immediately developed sneezing, runny nose and nasal congestion. These symptoms resolved quickly once the doctor revealed his deception to the patient.
Observations such as this stimulated interest in hypnosis as a possible treatment for allergies. In 1958, the prestigious medical journal The Lancet reported a case of a woman whose allergies were cured by hypnosis. But initial enthusiasm for this technique waned after other doctors were unable to replicate these results. Eventually, hypnosis was abandoned as a treatment for allergies.
Still, doctors continued to note a high incidence of apparently psychosomatic symptoms among allergic patients. In a British survey of more than 10,000 people conducted in the 1990s, for example, 20 percent indicated that they developed itching, hives and other allergic symptoms in response to various foods. But fewer than 2 percent reacted to these foods on formal skin testing.
Placebo studies have proved uniquely useful in differentiating psychic symptoms from allergic ones. In 2011, investigators studied the effect of placebo inhalers in patients with mild-to-moderate asthma, a condition that frequently coexists with allergies. They found that patients perceived the same degree of relief with the placebo inhaler as they did with the actual asthma inhaler. Yet, their lung function tests improved only with the active medication.
A 2018 German study confirmed the effectiveness of placebos in patients with allergic rhinitis, the medical name for hay fever. Allergic symptoms such as itching, sneezing and runny nose improved even though the patients were aware that they were receiving a placebo.
What is one to conclude from all these studies? First, while emotions and psychological stress do not cause allergies, they can worsen symptoms. Next, while mind-body techniques may be useful adjuncts in easing symptoms, they are not sufficient to treat the underlying problem. Finally, placebo studies show the physician-patient relationship itself can be therapeutic. Maintaining a close relationship with a doctor you like may be one of the best way to maximise the benefits of allergy drugs and therapies.